At Common Purpose we advise our clients to rest for a minimum of six weeks after birth. If the birth went without complication, then six weeks is the standard recovery time suggested by medical practitioners. If any surgical procedures (like a caesarean section) were performed, then doctors will usually suggest extending your recovery time to at least 8 weeks. These recommendations are general and individual’s recovery times will vary. But all this to say, don’t feel discouraged if you’re not back in the gym for at least two months after giving birth.
There are two important reasons why at least six weeks is recommended. Firstly, welcoming a new life into the world is an amazing and important part of your life that you’ll never get back, so we highly recommend you give yourself time to spend with your baby to connect with them, in all senses of the word.
Secondly, it must be understood that giving birth is traumatic (to say the least) and will create drastic changes within the body. Simply put, your body needs time to heal and recover. The majority of the trauma is internal and, unfortunately, it’s not unusual for medical procedures to be carried out in the process. It’s important to note that there will inevitably be scar tissue forming, which will be with you for life. For context, typical orthopaedic injuries take around 12 to 16 weeks to heal.
With all this in mind, it’s important to allow the body enough time to repair and recuperate. The priorities during the first six weeks are;
- Physically and emotionally recover from birth.
- Establish physical contact and emotional connection between the mother and baby.
- Establish new eating and sleeping patterns.
- Gentle movement (walk around the house with or without the baby).
- Start easy, low-level diaphragm-core-pelvic floor exercises in or beside the bed (if you have the energy or desire to do so!)
The Baby Blues and Postpartum Depression
The postpartum period is an inevitable rollercoaster of emotions. After such a life-changing experience, a huge shift in biological processes, routine and sleep (let alone being ultimately responsible for another life!), it’s common for postpartum mums to feel a bit down, tearful, or anxious in the first couple of weeks after giving birth;
“80% of women experience baby blues, 1 in 9 women experience postpartum depression” (1)
If the baby blues start to last longer than two weeks and/or start to get worse, then you may be experiencing postpartum depression. Here are some signs to look out for according to the NHS website (2);
- A persistent feeling of sadness and low mood.
- Lack of enjoyment and loss of interest in the wider world.
- Lack of energy and feeling tired all the time.
- Trouble sleeping at night and feeling sleepy during the day.
- Difficulty bonding with your baby.
- Withdrawing from contact with other people.
- Problems concentrating and making decisions.
- Frightening thoughts; about hurting your baby, for example.
It’s important to reach out to those close to you for help should you need it and this includes your doctor or midwife too.
Nutritional Tips
We gave the majority of our nutrition advice in the previous article “Pregnancy Exercise pt3: Nutrition Advice” and we’d encourage you to continue to follow the same healthy habits. The foods we eat are literally the building blocks the body uses to repair muscles and tissues, so try to revert back to your healthy habits as quickly as possible. However, there are a few things to know during the postpartum period that can help save precious time, reduce stress and support your body’s healing processes:
- Cook food in batches – Lasagnas, tray-bakes and slow-cooker recipes are all great ways to cook multiple meals that you can store in the fridge or freezer. Cooking multiple meals in one is a massive time saver.
- Buy healthy pre-prepared foods or ingredients that are pre-chopped and seasoned – again another time-saver in the long run.
- Outsource your cooking – Turning to family members or friends for some help in making some batch cooked food can really help. Also turning to a food delivery service that makes bespoke meals are really convenient and becoming more affordable.
- Order shopping online – it’s a simple suggestion but it will certainly save time.
- Slightly increase calorie intake (but don’t force it) – as mentioned in our previous article, an extra 500kcal a day whilst breastfeeding is recommended, but it’s important to listen to your body here as it’s likely your hunger will naturally increase anyway. Try and get these extra calories through healthy food sources (maybe add an extra healthy meal to your day).
- Stay away from alcohol – According to the Mayo Clinic, there is no safe level of alcohol a mother can drink during breastfeeding since alcohol consumed will be passed to the baby via the mother’s milk (3). Alcohol also decreases milk production and also the amount the baby drinks by about 20%. We’d advise you to err on the side of caution and remain teetotal whilst breastfeeding, however, we understand the choice is ultimately down to you. It’s relatively common to hear of people consuming infrequent, low levels of alcohol away from breastfeeding times and sometimes this helps following a long period of abstinence during pregnancy.
- Increase your calcium intake – Breast milk is rich in calcium and if a breastfeeding mother is deficient then her body will turn to her own calcium stores to ensure the baby gets enough (The National Academy of Sciences recommends that women who are pregnant or breastfeeding consume 1,000 mg (milligrams) of calcium each day). Dark leafy greens and dairy products are a great natural source of calcium however a good post-natal supplement will likely have increased levels of calcium too.
- Stay Well Hydrated – Due to the amount of fluid needed during breastfeeding, guidelines stipulate that 4ltrs of water is needed every day. We understand this is a lot, so use 4ltrs as a target but don’t let it stress you out too much if you come in just shy.
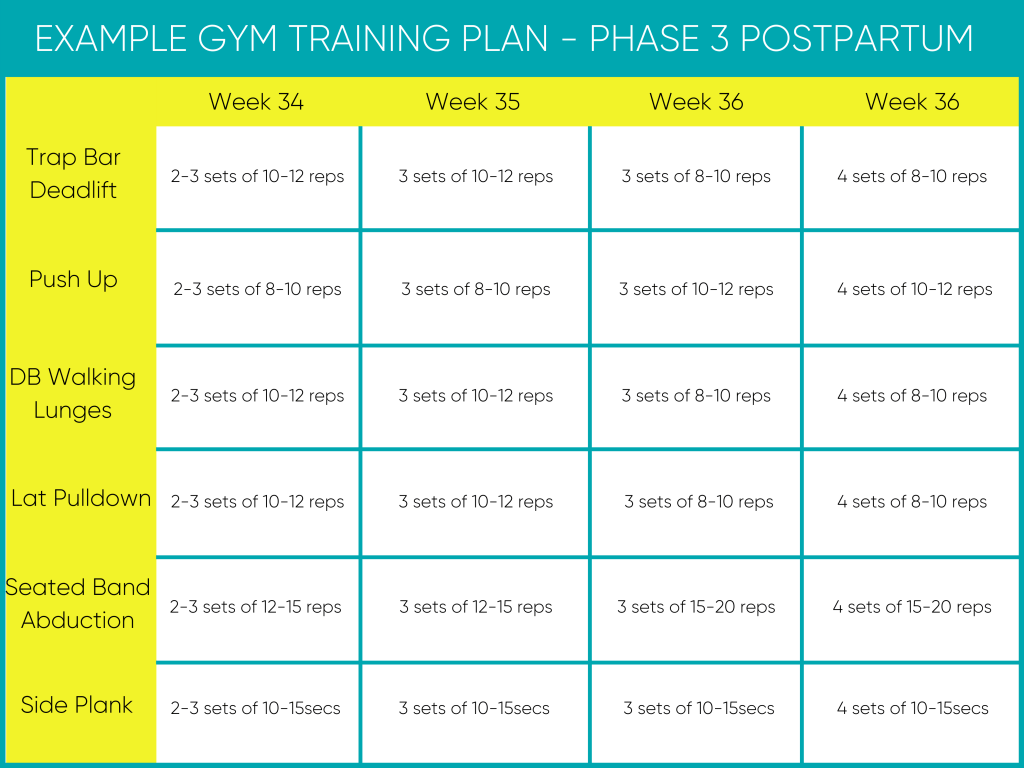
Phase 2 (7 to 18 weeks after birth) – Rebuild